About the Pulmonary Disease and Critical Care Medicine Fellowship Program
Fellows' Perspectives on the Program
“There are so many reasons that make fellowship enjoyable at VCU. My co-fellows and attendings are wonderful humans and clinicians - the atmosphere is always supportive and collegial. The amount of educational, clinical and research opportunities are abundant and allow each of us as fellows to pave our path for future careers.”
Meliha Hrustanovic-Kadic, MD - 2023
Welcome to the Pulmonary and Critical Care Medicine (PCCM) Fellowship program website. The fellowship is accredited by ACGME as a three-year combined program that provides state-of-the-art training in both pulmonary disease and critical care medicine. We are incredibly proud of our fellows and our program, and are fortunate to be part of an amazing Department of Internal Medicine and outstanding medical campus at VCU. Our fellows rotate through both the VCU Medical Campus, a quaternary academic medical center serving Virginia and the surrounding mid-Atlantic region, as well as the Richmond VAMC, a tertiary care VA hospital with a new state of the art ICU. Both campuses have advanced simulation facilities that supplement bedside training in bronchoscopy, airway management, bedside ultrasound, and critical care procedures.
Our fellows receive outstanding clinical and scholarly training in both pulmonary and critical care medicine, benefiting from direct experience, training, and mentorship in our comprehensive and advanced subspecialty programs including the Interventional Pulmonary Program, Pulmonary Hypertension Center of Excellence, Adult Cystic Fibrosis Program, Interstitial Lung Disease Program, Multisystem Sarcoid Clinic, and our Severe Asthma Clinic. Finally, our new Lung Transplantation Program is rapidly moving forward.
Our division has expanded the last few years under the leadership of Dr. Patrick Nana-Sinkam, adding new faculty in advanced ILD, interventional pulmonary, critical care medicine, ethics, pulmonary hypertension, lung cancer, advanced asthma, and lung transplantation. Similarly, our fellowship program has expanded from a total of 12 fellows (4 per year) to 15 fellows (5 per year). While that growth is exciting and has truly expanded the opportunities for our fellows, we have not lost what made us so special in the first place: a truly rich and diverse clinical experience with opportunities from research and mentorship all set in a rich, supportive, and diverse learning climate. Our fellows are indeed part of our division, and that collegiality remains a large part of who we are. It might also all add up to why both our fellows and our division consistently wins the department teaching awards year after year. We’re also extremely fortunate to have Dr. Patricia Sime, an internationally known and respected researcher in ILD, as our DOIM Chair and member of our division. Her leadership and strong support in innovation, service, education and research is inspiring.
Finally, all of this happens in the setting of a city increasingly recognized by Forbes, Lonely Planet, NY Times, US News and others as one of the top best places to live and visit. Marked by an affordable cost of living, diverse neighborhoods, a vibrant food and beverage scene, good weather and outstanding parks, Richmond is also a short day trip to the beach, the mountains and DC. It’s not hard to see why so many people fall in love with the city and never leave. We hope you’ll take a look and come join us.
The mission of the program is to ensure fellows:
- Develop an understanding of the scientific and clinical principles of pulmonary and critical care medicine.
- Develop the clinical and procedural skills required for the practice of pulmonary and critical care medicine through direct observation and management of both inpatients and outpatients with a variety of pulmonary disorders and critical care illness. There will be supervision and evaluation by qualified faculty in these encounters. The fellow will be given graded authority and responsibility based on their performance.
- Are exposed to opportunities in basic science and/or clinical research to foster better understanding of these fields and their integration in clinical practice and/or to develop a career in academic medicine.
- Have an environment that fosters practice-based learning and the development of leadership and teaching skills.
- Are instructed in and follow the principles of medical ethics and professionalism.
- Develop an understanding, awareness and responsiveness to the principles of systems-based practice.
Welcome
Program Director: Lisa K. Brath, MD
Learn
Program Curriculum & Conferences
Curriculum
Program Overview

The first year of fellowship is a clinical one, aimed at teaching fellows the basic aspects of pulmonary medicine and critical care medicine. Rotations therefore are primarily in the medical ICUs as well as the pulmonary consult services, including both general and interventional pulmonary, pulmonary hypertension and others. During this year, fellows identify and meet with mentors to help shape their fellowship path to meets their individual career aspirations.
The second and third years of fellowship are aimed at refining and expanding the knowledge gained during the first year and are structured to support the development of each fellow’s career interests. Elective time is used to gain more clinical experience outside the typical medical ICU or pulmonary consult setting, to gain research experience, and to pursue other scholarly projects. Fellows are also given the opportunity to pursue more dedicated clinical time in areas of interest, such as ILD or PH for example.
 The PCCM fellowship is a 3-year training program designed to satisfy the requirements for both the Pulmonary and Critical Care Medicine subspecialty board certification. More importantly though, the program is designed to prepare the fellow for a career in pulmonary and critical care medicine by provided state of the art clinical training, basic or clinical research opportunities, and teaching / leadership responsibilities. The structure ensures that the first year fellows gain a solid foundation in both fields that then allows each individual fellow to pursue a more refined, individualized educational experience during the second and third years of fellowship, adding in more elective and research time to create a more personalized roadmap for success. Inherent in all of our training is a commitment to excellence for each patient, regardless of their background and challenges. Our fellows come from all over the country and world, enriching our program with their diverse backgrounds and belief. They are a strong compliment to the diverse patient population we are humbled to serve.
The PCCM fellowship is a 3-year training program designed to satisfy the requirements for both the Pulmonary and Critical Care Medicine subspecialty board certification. More importantly though, the program is designed to prepare the fellow for a career in pulmonary and critical care medicine by provided state of the art clinical training, basic or clinical research opportunities, and teaching / leadership responsibilities. The structure ensures that the first year fellows gain a solid foundation in both fields that then allows each individual fellow to pursue a more refined, individualized educational experience during the second and third years of fellowship, adding in more elective and research time to create a more personalized roadmap for success. Inherent in all of our training is a commitment to excellence for each patient, regardless of their background and challenges. Our fellows come from all over the country and world, enriching our program with their diverse backgrounds and belief. They are a strong compliment to the diverse patient population we are humbled to serve.
Typical Rotation Schedules
Pulmonary Rotation Descriptions
Pulmonary Consults (VCUHS and McGuire VAMC)
The consult service both at VCU and the VA consists of a PCCM faculty and fellow as well as IM interns, residents and M4 students. The consult team sees all of the inpatient consults, performs inpatient and outpatient bronchoscopies, and interpret pulmonary function tests. The patients present with a broad range of both acute and chronic pulmonary medicine, ranging from typical breath and butter pulmonary medicine to the more complex, unusual cases typical of an advanced academic medical center. Our large referral base, safety net hospital status, and multiple solid organ and cellular/bone marrow transplant programs combine to provide a robust experience. The pulmonary consult service at the VA is also responsible for a large variety of complex, advance interventional pulmonary procedures. The consult service is covered by the ICU team nights and weekends.
Interventional Pulmonary (VCUHS)
Our IP program is the largest and most established program in the state, attracting referrals from across Virginia. Fellows are exposed to a wide variety of experiences and procedures including endobronchial ultrasound, rigid bronchoscopy, cryobiopsy, stent placement, laser, bronchial thermoplasty, pleuroscopy, navigational bronchoscopy, ultrasound guided thoracentesis, chest tube placement, endobronchial valve placement, and percutaneous tracheostomy. The VCU campus has three IP trained faculty and an established, successful IP fellowship. The VA has additional IP trained faculty, the only difference being that it is part of the general consult service. Between the two places, our fellows are able to get extensive, hands on experiences and develop competency in multiple advanced procedures.
Fellows' Perspectives on the Program
“We get a lot of procedural experience. Even on my first rotation on IP, when I hadn’t done any of it, every day I was doing procedures. You’re not just sitting in the background watching. First week you are up and doing them.”
Logan Rosenberg, MD - 2026
Pulmonary Hypertension
VCU is designated as a PHA Center of Comprehensive Care. The vast majority of PH clinical care and research occurs within our division, although we have an excellent relationship with our advance heart failure colleagues. Fellows work with designated PH faculty on both inpatient consults as well as the outpatient PH clinic. They also have the opportunity to do right heart caths during this rotation.
Adult Cystic Fibrosis
Similar to PH, fellows round on both the inpatient and outpatient CF services. The inpatients themselves are under the primary care of our general medicine teams, with the CF service serving in a co-management role.
Ambulatory Clinics
All fellows maintain a panel of patients in a general pulmonary clinic, seeing them ½ day per week all three years, splitting time between VCU and the VA. Both clinics are staffed by PCCM attendings. Fellows also rotate through the faculty clinics, including general pulmonary, ILD, advanced sarcoid, chest tumor, PH, CF, bone marrow transplant, and lung cancer screening to name a few.
Critical Care Rotation Descriptions
Fellows' Perspectives on the Program
The faculty are great. They really make you feel like you are a junior faculty, a part of the group, and definitely someone they are taking under their wing to help teach you all the things you need to know.
Perry Rabin, MD - 2026
MRICU (VCUHS)
The MRICU, or Medical Respiratory ICU, is a 28 to 36-bed unit located in our 11 story critical care tower. This is a closed unit staffed by 3 full teams. Two of the teams are classic housestaff teams, each including a PCCM attending and fellow, IM interns and residents, critical care PharmDs and nutritionists—a true multidisciplinary model. The third team is an APP/faculty model and is a great rotation for our third year fellows as part of their transition to practice. The unit is a very busy, urban ICU that receives admissions from our ED, multiple inpatient services and departments, and from referral hospitals throughout the state. The patients represent some of the most complex, acutely ill cases in the state, affording our fellows a tremendous educational experience. Fellows get extensive hands-on experience including ventilator and airway management, critical care ultrasound, percutaneous tracheostomy, and the management of severe multi-organ failure. We look to our fellows to take a progressive leadership role as they gain experience and knowledge, truly becoming independent critical care physicians. We utilize a night float system both for residents and fellows on this rotation.
MICU (VAMC)
The newly renovated VA MICU opened in April 2020. This state-of-the-art unit is home to 12 beds for MICU patients. The MICU team consists of a PCCM attending, PCCM fellow, IM residents, categorical interns, dieticians, and pharmacists. Call is from home with an IM resident in-house. Fellows are expected to be immediately available by phone and to go in for truly urgent needs.
CSICU (VCUHS)
We are fortunate to have a very active and aggressive cardiothoracic surgery program. Our patients benefit from many exciting clinical programs including minimally invasive surgical techniques for valvular heart disease, heart transplantation, and surgical approaches to cardiac arrhythmias. The CSICU is a co-management type model, and our fellows rotate with the critical care team, helping to manage these postoperative patients as well as those who require ventricular assist devices, total artificial hearts and ECMO. Fellows typically rotate through here during their second/third years.
STICU (VCUHS)
VCU Medical Center is the primary comprehensive Level I adult, pediatric, and burn trauma center in the region. The STICU, or Surgery Trauma ICU, is a 28-bed unit that provides comprehensive care to a diverse population of severely injured and critically ill surgical patients. The unit has two primary intensivist-led services: the trauma ICU, a closed service staffed by trauma/critical care surgeons and intensivists, and the surgical ICU, which is co-managed by intensivists and attending physicians. Physicians represent a breadth of fields including these surgeries: acute general, burn, minimally invasive, colorectal, orthopedic, plastic, otolaryngology and oncology. Fellows typically rotate through here during their second/third years.
NSICU (VCUHS)
The NSICU, or Neuroscience Intensive Care Unit, is an 18-bed unit specializing in the treatment of patients who have suffered from stroke, traumatic brain injury, spinal cord injury and other neurological and neurosurgical conditions. NSICU clinical services include patient care by neurosurgical and neurology physicians using a co-management model with the intensivist service. Fellows typically rotate through here during their second/third years.
CICU (VCUHS)
The CICU, or Cardiac Intensive Care Unit, is a 14-bed closed ICU staffed by the Division of Cardiology. The CICU serves patients with acute coronary syndromes such as myocardial infarction and unstable angina, cardiogenic shock, congestive heart failure, pulmonary edema, cardiac arrest and dysrhythmia. The unit cares for critically ill patients following cardiac catheterization, percutaneous coronary interventions, pacemaker insertion and cardiac defibrillator implants. In addition to standard ICU therapies, the CICU also provides specialty therapies for ECMO, TAVRs, hypothermia, temporary pacemakers, intra-aortic balloon pumps and pulmonary artery catheters. Fellows typically rotate through here during their second/third years.
Electives
- Sleep Medicine
- Ultrasound
- Thoracic Radiology
- Thoracic Surgery
- Ambulatory clinics
- Pulmonary rehab and cardiopulmonary exercise testing
- Respiratory therapy and PFT lab
- Anesthesia
- Other: ENT, allergy, infectious disease, bone marrow transplant, private practice, lung transplant, advanced ILD, rapid response, global health.
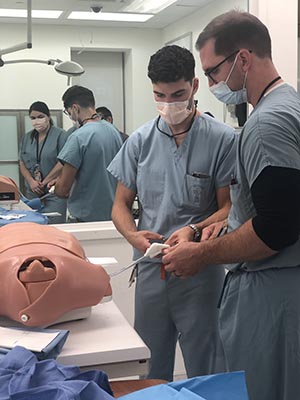
Simulation Center Activities
- Airway management
- ACLS Team-based Training
- Critical Care Ultrasound, both basic and advanced
- Bronchoscopy simulation
- Critical Care procedures
Conferences
Conferences
Boot camp
A 2-week introduction to fellowship that includes extensive procedural training in the simulation center (common ICU procedures, bronchoscopy, ultrasound, airways) as well as topics including leadership in the ICU and on the consult team, how to be an effective teacher, etc. This also starts the summer basics didactic series.
Core Curriculum
A weekly, one-hour didactic format covering major topics from the ABIM Blueprint for both pulmonary and critical care focusing on high yield pearls in pathophysiology, epidemiology, diagnosis, prognosis, and management; pertinent updates in the literature; and if appropriate to the topic, highlight rarer presentations/diagnoses that fellows are unlikely to encounter in clinical practice to supplement training. These conferences are all given by faculty.
Physiology
Monthly case-based applied physiology conference centered around both West and Lange Pulmonary Physiology as well as other resources.
Journal Club
A quarterly conference typically held off campus at one of the local breweries and/or restaurants. It’s a great opportunity to combine an educational event with some of what RVA has to offer.
MMI
A quarterly morbidity, mortality and improvement conference.
Diagnostic Reasoning/Ambulatory Curriculum
A case-based conference with input from key faculty.
Chest Radiology Conference
A weekly conference with our Thoracic Radiology Division and includes core lectures by Thoracic Radiology Faculty and a case-based unknown style presentation by fellows.
ILD Conference
Monthly multidisciplinary conference led by our ILD group along with Thoracic Radiology and Surgical Pathology.
HALO Conference
This is a hands-on, skills-based conference held in the SOM simulation lab focused on High Acuity Low Occurrence events. Placement of bronchial blockers is one example covered in this series.
Pulmonary Grand Rounds
A bimonthly conference that brings in speakers from throughout VCU as well as other institutions.
Ultrasound
Our ultrasound curriculum starts with a 2-day CME style conference in July, modeled after the ACCP/CHEST Critical Care Ultrasound Course, and typically includes trainees and faculty from across the region. Two of our faculty members, Drs. Sammy Pedram and Peter Lee are instructors for the ACCP/CHEST national courses. We also bring in our talented and enthusiastic Emergency Medicine colleagues, namely the key leaders of their Ultrasound Fellowship. The curriculum then continues monthly throughout the year, combining both image interpretation and acquisition sessions. Images are submitted for review through our Q-Path system. Fellows will also spend 2 weeks rotating with the EM Ultrasound Fellowship Program.
Airway Management
This year long curriculum is a combination of both didactic and hands on experiences, that begins with basic anatomy and pharmacology and advances to techniques needed for the difficult airway.
Ethics/Palliative Conference
We are fortunate to have faculty who have additional training in both bioethics and palliative medicine to lead this case-based conference series in which we explore the principles of bioethics and palliative medicine.
Procedural Simulation Training
We are fortunate to have two state-of-the-art simulation centers, including one in the VCU School of Medicine and one at the VAMC. Both offer state of the art simulation models for invasive procedures including central line insertion, paracentesis, thoracentesis, chest tube insertion, lumbar puncture, etc. Both places also have advance bronchoscopy simulators, code simulators, advanced airway simulation mannequins and ultrasound simulation models.
Scholarship
Our recent publications, presentations and abstracts
Fellows' Perspectives on the Program
“This is wonderful place to get your career started, to have the mentorship from a faculty who are really invested in your education and career path.”
Jared Dyer, DO - 2023
All fellows are expected to actively engage in scholarly activities. These activities can be in basic research, translational research, clinical research, health outcomes research, and/or educational research. Essential to success is providing the tools necessary to foster the fellows’ intellectual development as investigators. As a sign of our commitment to the scholarly efforts of the fellows, the Department of Internal Medicine has designated funding which is set aside specifically to offset the travel cost for fellows who are presenting their work at regional, national, and international scientific and academic meetings.
Katlyn Baxter, DO
- Baxter K, Syed A. Sepsis causing spirochete leading to diffuse alveolar hemorrhage, acute renal failure & jaundice. CHEST international conference. October 2020.
-
Baxter K, Kashiouris M, Qayyum R, Masters H, et al. Changes in the Hospital Medicine Service (HMS) Admitting Practices Decreased the Medical Intensive Care Unit (ICU) Boarding Time and Hospital Length of Stay. Accepted for poster presentation. ATS international conference. May 2020.
Jared Dyer, DO
-
Dyer J, Grinnan D, Kashiouris M, Sonntag E. RAPID RESPONSE AND THE CARE OF INPATIENT PULMONARY ARTERIAL HYPERTENSION PATIENTS. CHEST. April 2021.
-
Dyer J, Potfay R. DEATH BY CHYLOTHORAX. CHEST. October 2021.
Masoud Faridnia, MD
-
Skummer P, Kobayashi K, Schoeneck M, Patel J, Faridnia M. Single-session versus two-session placement of chest port and gastrostomy tube in patients with head and neck cancer: Is there any difference in the device-related early infection rates? Acta Radiologica Open, August 2021 10(8).
-
Patel S, Siddiqui MB, Roman JH, Zhang E, Lee E, Shen S, Faridnia M, Mintini RJ, Boyett S, Idowu MO, Sanyal AJ, Luketic VA, Siddiqui MS. Association Between Lipoprotein Particles and Atherosclerotic Events in Nonalcoholic Fatty Liver Disease. Clinical Gastroenterology Hepatology, October 19, 2021 (10): 2202-2204.
Rachel Gunthrie, MD
-
Guthrie R. Chronic Cough: Common Complaint with an Uncommon Diagnosis. Poster Presentation. American College of Chest Physicians. October 2019.
-
E. Gershman, R. Guthrie, K. Swiatek, S. Shojaee. Management of hemoptysis in patients with lung cancer. Ann Transl Med. 2019 Aug;7(15):358. doi: 10.21037/atm.2019.04.91. Published
-
Grinnan D, Guthrie R, L’Heureux M, Swiatek K. Beyond the Blue: What Fellows are Reading in Other Journals; Pulmonary Hypertension: Advances in Risk Assessment and Emerging Procedures. AJRCCM 2020. Accepted for publication.
-
Guthrie, R., Moses, L. Unexplained Cough, Dyspnea, and Eosinophilia: Don’t Forget the Zebras. Poster Presentation. American Thoracic Society National Meeting.
-
Gershman, E., Guthrie, R., Swiatek, K., Shojaee, S. Management of hemoptysis in patients with lung cancer. Annals of Translational Medicine, April 2019. Published.
Meliha Hrustanovic-Kadic, MD
1. Hrustanovic-Kadic M, Ziegler C, El-Kersh K. Palliative Care Perception in Pulmonary Arterial Hypertension: Evaluating the Interaction of PPCI, PAH-SYMPACT Questionnaire, and the REVEAL 2.0 Risk Score. Annals of the ATS.
George Kallingal, DO, PhD
-
Kallingal G. Complications Associated with Serial Thoracentesis in Cirrhotic Patients with Hepatic Hydrothorax. Oral Abstract. CHEST. October 2016. Los Angeles California.
-
Forbes, K., Kallingal G., Krones, A., Doern, C., Syed, A. Pneumonia Pathogen Identification Improves with Bedside Plating of Bronchoalveolar Lavage Fluid. Poster Presentation. 15th Annual VCU Resident & Fellow Research Day.
-
Bharara, A., Kallingal, G., Potfay, R. It is Not Called Crypto For Nothing. Poster Presentation. 2017 CHEST conference.
-
Schneider, E. Kallingal G., Miller, K., Kashioris, M. Safety of ABCDEF Bundle Implementation in a Medical ICU. Poster Presentation. 2017 CHEST conference.
-
Shojaee, S., Khalid, M., Kallingal G., Kang, L., Rahman, N. Repeat Thoracentesis in Hepatic Hydrothorax and Non-hepatic Hydrothorax Effusions: A Case Control Study. Peer-Reviewed Publication. Respiration. Accepted.
Michael L’Heureux, MD
-
L'Heureux M, Kashiouris M, Fowler A, Fisher B. Association Between IL-10 and Mortality in Sepsis-Induced ARDS. American College of Chest Physicians. October 2020.
-
L'Heureux M, Swiatek K, Guthrie R, Brath L, Grinnan D. Pulmonary Hypertension: Advances in Risk Assessment and Emerging Procedures. American Journal of Respiratory and Critical Care Medicine.
-
L’Heureux M, Grinnan D. “Holey Heart: Fistulizing Staphylococcal Endocarditis.” Poster Presentation. CHEST. October 2019.
-
Kashiouris, M.G.; L’Heureux, M.; Cable, C.A.; Fisher, B.J.; Leichtle, S.W.; III, A.A.F. The Emerging Role of Vitamin C as a Treatment for Sepsis. Nutrients 2020, 12, 292.
-
L’Heureux, M., Sternberg, M., Brath, L. et al. Sepsis-Induced Cardiomyopathy: a Comprehensive Review. Curr Cardiol Rep 22, 35 (2020). https://doi.org/10.1007/s11886-020-01277-2.
-
Grinnan D, Guthrie R, L’Heureux M, Swiatek K. Beyond the Blue: What Fellows are Reading in Other Journals; Pulmonary Hypertension: Advances in Risk Assessment and Emerging Procedures. AJRCCM 2020. Accepted for publication.
-
L'Heureux, M., Grossman, C., Porter, C., Iden, T., Potfay, R. Multimodal Needs Assessments for Curricular Refinement - Learner, Expert, EMR. VCU Health Sciences Education Symposium. March 2019.
-
L'Heureux, M., Miller, R., Call, S. Immersion in Physiology Bolsters Mechanistic Thinking. VCU Health Sciences Education Symposium. March 2019.
Kathryn Logothetis, MD
1. Logothetis K, Pillappa R, Robila V, Li H, Lee P. Primary Pulmonary Myxoid Sarcoma: A Rare Cause of Hemoptysis. American Thoracic Society. May 2021.
Andrew MacMillan, DO
-
MacMillan A. Diffuse Idiopathic Pulmonary Neuroendocrine Cell Hyperplasia: A Rare Clinical Disorder. Poster presentation. CHEST 2020.
-
MacMillan A. African American Patients with COVID-19 Experience Longer Hospital Length of Stay Compared with the Other Patients: An Epidemiological Study of 583 US Hospitals. Poster presentation. ATS. May 2021.
Jessica McLaughlin, DO
- McLaughlin J. A Case of Xanthoma Disseminatum in the Trachea. Poster Presentation. ATS International Conference. May 2022.
Sarah Morgan, MD
-
Morgan, S. Fever in ICU. Critical Care Case Files. Published.
Sean Murney, MD
-
Murney S, Radchenko C, Shepherd R. Unrelenting Tracheobronchial Stenosis in Relapsing Polychondritis. Thematic Poster. ATS, May 2018.
-
Murney S, Syed A, Doern C. Pneumonia Pathogen Identification in Bronchoalveolar Fluid: Use of a Multiplex PCR Test Compared with Bedside Plating. Poster Presentation, Abstract Accepted. ATS, May 2020.
Andrea Mytinger, MD
-
Mytinger A. Tricuspid and Pulmonary Valves Resembling Carcinoid Heart Disease in Methamphetamine-Associated Pulmonary Arterial Hypertension. Poster Presentation. CHEST. October 2019.
-
Mytinger A. Amiodarone-Induced Pneumonitis: Wait and C. Poster Presentation. CHEST. October 2019.
-
Mytinger A, Taylor T, E. Gershman, Shojaee S. Recommended Reading from the Virginia Commonwealth Pulmonary/Critical Care and Interventional Pulmonary Fellows. Am J Respir Crit Care Med. 2020 May 18. doi: 10.1164/rccm.202003-0599RR. Published
Zulma Swank, DO
-
Swank Z. Interstitial Lung Disease in sub-Saharan Africa. ATS. May 2021.
-
Swank Z. Improvised T-tube for Management of Cotton-Myer Grade IV Subglottic Stenosis. CHEST. October 2020.
-
Matta A, Gupta E, Swank Z, Aragaki-Nakahodo A, Cooley J, Caudell-Stamper DN, Benzaquen S. The use of transbronchial cryobiopsy for diffuse parenchymal lung disease in critically ill patients with acute hypoxemic respiratory failure-A case series. Clinical Respiratory Journal, March 2021. Published.
-
Liu H., Osterburg A., Flury J., Swank Z. MAPK Mutations and Cigarette Smoke Promote the Pathogenesis of Pulmonary Langerhans Cell Histiocytosis. JCI Insight. 2020; 5(4): e132048. doi.org/10.1172/jci.insight.132048. Published
-
Cooley J, Swank Z, Baughman R, Benzaquen S. Safety of Performing Transbronchial Lung Cryobiopsy on Hospitalized Patients with Interstitial Lung disease. Respiratory Medicine. 2018; 140: 71-76. doi: 10.1016/j.rmed.2018.05.019.
Kevin Swiatek, DO
-
Sonntag E, Orme-Evans G, Swiatek K, Hunsucker M, Ferre Martinez J, Minai S, Grinnan D, Ford H, Pinson J, Lester C, Glover B, Levarge B. End of Life Needs and Preferences in Patients with Pulmonary Arterial Hypertension. American Thoracic Society.
-
Swiatek K, Lester C, Ng N, Golia S, Pinson J, Grinnan D. Impact of Face Masks on 6-Minute Walk Test in Healthy Volunteers. Pulmonary Circulation, 2021.
-
Swiatek KM, Potfay R. Exception to the Rules: An Incidental Finding of Pulmonary Artery Dissection During EBUS. Abstract accepted. Am. Jr. of Respiratory and Critical Care Medicine. 2020
-
Mytinger A, Swiatek KM, Grinnan D. Tricuspid and Pulmonary Valves Resembling Carcinoid Heart Disease in Methamphetamine-Associated Pulmonary Arterial Hypertension. Abstract. Chest, 2019, 156(4). doi: 10.1016/j.chest.2019.08.534
-
Swiatek KM, Mytinger A, Grinnan D. Use of Riociguat to Liberate from Prolonged Use of Inhaled Nitric Oxide in the Intensive Care Unit. Case Reports In Pulmonary Vascular Medicine Ii. 2019. doi: 10.1164/ajrccm-conference.2019.199.1_meetingabstracts.a3597
-
Swiatek KM, Guthrie R, L’Heureux M, Grinnan D,. Beyond the Blue: What Fellows are Reading in Other Journals. Pulmonary Hypertension: Advances in Risk Assessment and Emerging Procedures. Accepted for publication. Am. Jr. of Respiratory and Critical Care Medicine. 2020.
-
Swiatek KM, Pedram S. (2020) Critical Care Echocardiography: 1000 Questions and Answers. Chapter 56: Differentiating Pulmonary Edema, Pneumonia, COPD/Asthma, Bronchiolitis, ARDS, Pulmonary embolism. Wolters Kluwer. Publication Accepted.
-
Swiatek, K. Use of Riociguat to Liberate from Prolonged Use of Inhaled Nitric Oxide in the Intensive Care Unit. American Thoracic Society National Meeting. May 2019.
-
Swiatek, K. An Unlikely Presentation of Fat Embolism Syndrome. American College of Chest Physicians Annual Meeting 2018.
-
Gershman, E., Guthrie, R., Swiatek, K., Shojaee, S. Management of hemoptysis in patients with lung cancer. Annals of Translational Medicine, 2019. Accepted.
Trevor Taylor, MD
-
Mytinger A, Taylor T, E. Gershman, Shojaee S. Recommended Reading from the Virginia Commonwealth Pulmonary/Critical Care and Interventional Pulmonary Fellows. Am J Respir Crit Care Med. 2020 May 18. doi: 10.1164/rccm.202003-0599RR. Published
-
Sindel A, Taylor T, Chesney A, Clark W, Fowler AA 3rd, Toor AA. Hematopoietic stem cell mobilization following PD-1 blockade: Cytokine release syndrome after transplantation managed with ascorbic acid. Eur J Haematol. 2019;103(2):134‐136. doi:10.1111/ejh.13248.
Life During Fellowship
Pulmonary Disease & Critical Care Fellowship
 It goes without saying that a Pulmonary and Critical Care Fellowship is a demanding three years. But it also goes without saying that we are committed to your well-being, resilience and all aspects of a healthy lifestyle. Without a visit, it’s difficult to really grasp the fun and the camaraderie that our division is known for and compliments our dedication to education, patient care and scholarship. I’m convinced it is part of the reason we have been recognized as the best teaching division for too many years to count. We’ve worked hard to create a schedule that balances work and life, maximizing weekends off to enjoy all that Richmond and the region have to offer. As is typical, we offer 3 weeks paid vacation plus 5 days over the winter holidays and time off for conference attendance.
It goes without saying that a Pulmonary and Critical Care Fellowship is a demanding three years. But it also goes without saying that we are committed to your well-being, resilience and all aspects of a healthy lifestyle. Without a visit, it’s difficult to really grasp the fun and the camaraderie that our division is known for and compliments our dedication to education, patient care and scholarship. I’m convinced it is part of the reason we have been recognized as the best teaching division for too many years to count. We’ve worked hard to create a schedule that balances work and life, maximizing weekends off to enjoy all that Richmond and the region have to offer. As is typical, we offer 3 weeks paid vacation plus 5 days over the winter holidays and time off for conference attendance.
GME Resident & Fellow Well-Being
Graduate Medical Education training is not easy. With the GME Physician Well-being program, we first and foremost assert our commitment to your well-being, resilience and all aspects of a healthy lifestyle. VCU and VCUHealth are dedicated to ensuring that you have the tools you need to be your best. (Learn more)
All About VCU, VCU Health, and RVA
First things first. We fondly refer to Richmond as RVA. People love this city because it’s awesome. And Virginia Commonwealth University is in the middle of it all. Learn more about VCU, VCU Health, and RVA!
Program Leadership
Pulmonary Disease and Critical Care Fellowship

Lisa K. Brath, MD
Program Director

Lisa K. Brath, MD
Program Director
Internal Medicine
Division of Pulmonary Disease and Critical Care Medicine
Email: lisa.brath@vcuhealth.org
Jared Dyer, DO
Associate Program Director
Jared Dyer, DO
Associate Program Director
Department of Internal Medicine
Division of Pulmonary Disease & Critical Care Medicine
Email: jared.dyer@vcuhealth.org

Michael L'Heureux, MD
Associate Program Director

Michael L'Heureux, MD
Associate Program Director
Department of Internal Medicine
Division of Pulmonary Disease & Critical Care Medicine

Daniel C. Grinnan, MD
Interim - Division Chief

Daniel C. Grinnan, MD
Interim - Division Chief
Internal Medicine
Division of Pulmonary Disease and Critical Care Medicine
Email: daniel.grinnan@vcuhealth.org
Faculty
Pulmonary Disease and Critical Care Fellowship
VCU Faculty
- Farrukh Abbas, MD
- Lisa K. Brath, MD - Fellowship Program Director
- Casey Cable, MD
- Nauman A. Chaudary, MD, FACP, FCCP
- Marjolein de Wit, MD
- Jared Dyer, DO - Fellowship Associate Program Director
- Alpha A. Fowler, MD
- Daniel C. Grinnan, MD - Interim-Division Chief
- Catherine E. Grossman, MD
- Thomas Iden, MD
- Peter Jackson, MD
- Danai Khemasuwan, MD
- Michael L’Heureux, MD - Fellowship Associate Program Director
- Jessica McLaughlin, DO
- Kristin B. Miller, MD
- Patrick Nana-Sinkam, MD
- James O'Connor, MD
- Vipul Patel, MD
- Sammy Pedram, MD
- Apostolos Perelas, MD
- R. Wesley Shepherd, MD
- Patricia Sime, MD, FRCP - Department Chair
- Liz Sonntag, MD
- Aamer Syed, MD
- Toribiong, Uchel, MD
- Robert Winn, MD - Director, Massey Cancer Center
VAMC Faculty
- Seth E. Brant, MD - Section Chief
- Masoud Faridnia, MD
- Timothy Fusiak, DO
- Adam Kaiser, MD
- Benjamin Morang, DO
- Rebecca Potfay, MD
Fellows
Pulmonary Disease and Critical Care Fellowship
Class of 2028

Kate Boylan, DO
Medical School: Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Residency: Summa Health System, Akron, OH

Ali Khreisat, MD
Medical School: University of Jordan Faculty of Medicine, Amman, Jordan
Residency: Corewell Health William Beaumont University Hospital, Royal Oak, MI

Hiral Patel, DO
Medical School: Philadelphia College of Osteopathic Medicine, Philadelphia, PA
Residency: Prisma Health/University of South Carolina School of Medicine, Greenville, SC

Juhie Patel, DO
Medical School: Liberty University College of Osteopathic Medicine, Lynchburg, VA
Residency: Christiana Core Health Systems, Newark, DE

Jonathan Stewart, DO
Medical School: Philadelphia College of Osteopathic Medicine, Philadelphia, PA
Residency: Virginia Commonwealth University, Richmond, VA
Class of 2027

Alicia Brunelle, MD
Medical School: University of Massachusetts Medical School, Worcester, MA
Residency: University of Massachusetts Internal Medicine, Worcester, MA

Maged Elhaddah, MBBCh
Medical School: Ain Shams University Faculty of Medicine, Cairo, Egypt
Residency: MedStar Health, Columbia, MD

Jason Pecorella, MD
Medical School: University of South Carolina School of Medicine, Columbia, SC
Residency: Virginia Commonwealth University, Richmond, VA

Shruthi Sreekumar, MD
Medical School: West Virginia University School of Medicine. Morgantown, WV
Residency: University of Cincinnati Medical Center, Cincinnati, OH

Abdul Wahab, MBBS
Medical School: King Edward Medical University, Lahore, Pakistan
Residency: Rochester Regional Health/Unity Hospital, Rochester, NY
Class of 2026

Peter B Lowery, MD
Medical School: University of Arkansas for Medical Sciences, Little Rock, AR
Residency: Louisiana State University Health Sciences Center, New Orleans, LA

Jon Brandon (JB) Mullholand, MD
Medical School: Geisinger Commonwealth School of Medicine, Scranton, PA
Residency: Penn State Milton S Hershey Medical Center, Hershey, PA

Perry Rabin, MD
Medical School: Indiana University School of Medicine, Indianapolis, IN
Residency: Rush University Medical Center, Chicago, IL

Logan Rosenberg, MD
Medical School: University of Queensland School of Medicine – Ochsner Cohort, Herston, Australia
Residency: Legacy Emanuel/Good Samaritan, Portland, OR

Alisha Sharma, MD
Medical School: St. George’s University School of Medicine, Grenada
Residency: Allegheny Health Network, Pittsburgh, PA

Nathaniel Warner, MD
Medical School: Virginia Commonwealth University School of Medicine, Richmond, VA
Residency: Virginia Commonwealth University, Richmond, VA
Alumni
Class of 2025
Yussef Al Ghoul, MB ChB
Medical School: University of Benghazi Faculty of Medicine, Benghazi, Libya
Residency: University at Buffalo, Buffalo, NY
Heloisa DeCarvalho, MD
Medical School: Boston University School of Medicine, Boston, MA
Residency: Virginia Commonwealth University Health System, Richmond, VA
Catherine Jeeyoon Kim, DO
Medical School: Philadelphia College of Osteopathic Medicine, Philadelphia, PA
Residency: University of Florida, Gainesville, FL
Ashley Nicole Reluzco, MD
Medical School: Medical University of South Carolina College of Medicine, Charleston, SC
Residency: Medical University of South Carolina, Charleston, SC
Darryn Leslie Winter, DO
Medical School: Michigan State University College of Osteopathic Medicine, East Lansing, MI
Residency: Prisma Health/University of South Carolina School of Medicine, Greenville, SC
Class of 2024
Masoud Faridnia, MD
Medical School: State University of New York Upstate Medical University, Syracuse, NY
Residency: Virginia Commonwealth University Health System, Richmond, VA
Kathryn Ann Hess, MD
Medical School: Tufts University Maine Medical Center, Boston, MA
Residency: Virginia Commonwealth University Health System, Richmond, VA
Robert Edward Hosse, MD
Medical School: Louisiana State University School of Medicine, New Orleans, LA
Residency: LSU, Baton Rouge, LA
Behram Khan, MBBS
Medical School: University of Queensland School of Medicine, Herston, Australia
Residency: Ochsner Clinic Foundation, Covington, LA
Jessica McLaughlin, DO
Medical School: Edward Via College of Osteopathic Medicine, Blacksburg, VA
Residency: Inova Fairfax Medical Campus, Fairfax, VA
Class of 2023
Jared Dyer, DO
Medical School: Virginia Commonwealth University, Richmond, VA
Residency: Virginia Commonwealth University, Richmond, VA
Jason Frisbee, DO
Medical School: West Virginia School of Osteopathic Medicine, Morgantown, WV
Residency: University of Tennessee Medical Center, Knoxville, TN
Meliha Hrustanovic-Kadic, MD
Medical School: University of Louisville School of Medicine, Louisville, KY
Residency: University of Louisville School of Medicine, Louisville, KY
Michael Nguyen, MD
Medical School: Northeast Ohio Medical University, Rootstown, OH
Residency: Summa Health System, Akron, OH
Thomas Rusher, MD
Medical School: University of North Carolina School of Medicine, Chapel Hill, NC
Residency: Tulane University, New Orleans, LA
Class of 2022
Angelique Gross, MD
Medical School: Mercer University School of Medicine, Macon, GA
Residency: Virginia Commonwealth University, Richmond, VA
Kathryn Britt Logothetis, MD
Medical School: University of South Carolina School of Medicine, Columbia, SC
Residency: Virginia Commonwealth University, Richmond, VA
Andrew MacMillian, DO
Medical School: Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Residency: Riverside Methodist Hospitals, Columbus, OH
Mario Montalvo, DO
Medical School: Edward Via College of Osteopathic Medicine, Virginia Campus, Blacksburg, VA
Residency: Drexel University College of Medicine/Hahnemann University Hospital, Philadelphia, PA
Zulma Swank, DO
Medical School: Edward Via College of Osteopathic Medicine, Virginia Campus, Blacksburg, VA
Residency: University of Cincinnati College of Medicine, Cincinnati, OH
Class of 2021
Katlyn Baxter, DO
Medical School: Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Residency: Riverside Methodist Hospital, Columbus, OH
Michael Jerome L’Heureux, MD
Medical School: Virginia Commonwealth University School of Medicine, Richmond, VA
Residency: Virginia Commonwealth University, Richmond, VA
Andrea Katherine Mytinger, MD
Medical School: Western University of Health Sciences/College of Osteopathic Medicine of the Pacific, Pomona, CA
Residency: University of New Mexico Hospital, Albuquerque, NM
Kevin Michael Swiatek, DO
Medical School: Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Residency: Riverside Methodist Hospital, Columbus, OH
Class of 2020
Medical School: Virginia Commonwealth University School of Medicine, Richmond, VA
Residency: University of Maryland, College Park, MD
Medical School: Edward Via College of Osteopathic Medicine, Blacksburg, VA
Residency: Riverside Methodist Hospitals (OhioHealth) - Blacksburg, VA
Medical School: Lake Erie College of Osteopathic Medicine - Erie, PA
Residency: Riverside Methodist Hospitals (OhioHealth) - Blacksburg, VA
Medical School: Wake Forest University School of Medicine, Winstom-Salem, NC
Residency: Vanderbilt University Medical Center, Nashville, TN
Class of 2019
Medical School: Virginia Commonwealth University School of Medicine, Richmond, VA
Residency: Rutgers New Jersey Medical School, Rewark, NJ
Medical School: University of Illinois College of Medicine, Chicago, IL
Residency: University of Illinois College of Medicine, Chicago, IL
Medical School: Virginia Commonwealth University School of Medicine, Richmond, VA
Residency - Virginia Commonwealth University Health System, Richmond, VA
Medical School: University of South Carolina School of Medicine, Columbia, SC
Residency: Sidney Kimmel Medical College/Christiana Care Health System, Newark, DE
Class of 2018
Grant Farr, DO
Medical School: Des Moines University College of Osteopathic Medicine, Des Moines, IA
Residency: Virginia Commonwealth University, , Richmond, VA
George Kallingal, DO, PhD
Medical School: Lake Erie College of Osteopathic Medicine, Erie, PA
Residency: Riverside Methodist Hospitals, Blacksburg, VA
Erica Schneider, MD
Medical School: Louisiana State University School of Medicine, Baton Rouge, LA
Residency: Louisiana State University, LSU Health Sciences Center, Baton Rouge, LA
Megan Sisk, DO
Medical School: Kansas City University of Medicine and Biosciences College of Osteopathic Medicine, Kansas City, MO
Residency: Providence Hospital and Medical Centers Program, Irvine, CA
Class of 2017
Amit Bharara, MD
Medical School: University of Alabama in Birmingham School of Medicine, Birmingham, AL
Residency: Virginia Commonwealth University, Richmond, VA
Anand Pariyadath, MD
Medical School: Medical University of South Carolina, Charleston, SC
Residency: Virginia Commonwealth University, Richmond, VA
Katherine Price, MD
Medical School: Virginia Commonwealth University, Richmond, VA
Residency: Virginia Commonwealth University, Richmond, VA
James Pellerin, MD
Medical School: Virginia Commonwealth University, Richmond, VA
Residency: Virginia Commonwealth University, Richmond, VA
Class of 2016
Vikas Goyal, MD
Medical School: University of Texas Medical School, Austin, TX
Residency: Virginia Commonwealth University, Richmond, VA
Adam Kaiser, MD
Medical School: Louisianna State University Medical School, Baton Rouge, LA
Residency: Virginia Commonwealth University, Richmond, VA
Kristyn Sayball, DO
Medical School: Philadelphia College of Osteopathic Medicine, Philadelphia, PA
Residency: Virginia Commonwealth University, Richmond, VA
John Sentz, DO
Medical School: Edward Via Virginia College of Osteopathic Medicine, Blacksburg, VA
Residency: Virginia Commonwealth University, Richmond, VA
Apply
Pulmonary Disease and Critical Care Fellowship
Eligibility Requirements
The applicant should be an MD, DO, or MBBS with three or more years of Internal Medicine residency training in an ACGME-accredited training program. A pass on USMLE Step 3 is a mandatory prerequisite for acceptance as a fellow.
How to Apply
The Pulmonary Critical Care Medicine fellowship training program at VCU is a participant in the NRMP match. All applications will be accepted through ERAS and follow ERAS deadlines.
Required Documentation
- Application
- Curriculum Vitae
- USMLE score reports
- Medical school transcripts
- MPSE
- A personal statement
- 4 letters of recommendation, including one from your program director
- A photograph
If applicable, please provide the following:
- ECFMG certificate
- Medical School Diploma (with translation if necessary)
Application Timeline
We will review applications from July 15 through August 31. Invitations to interview will likely be issued during this time frame.
Interview Information
We typically interview in September and early October, Monday, Wednesday, Friday. Our day typically runs from 7:30-1pm with the following activities:
- Attend one of our weekly educational conferences
- Program overview with fellowship PD
- Interview with several faculty members
- Informal meet and greet with the fellows
Attention: In response to the COVID-19 pandemic and changes that followed, we like other programs shifted to a virtual interview format. This also had clear benefits for applicants with respect to time and cost. At this point, we plan to follow our national program directors association’s recommendation to continue this practice.
Contacts
Pulmonary Disease and Critical Care Fellowship
Program Director
Lisa K. Brath, M.D.
Box 980050
Richmond, Virginia 23298-0050
Phone: (804) 828-9071
Email: lisa.brath@vcuhealth.org
Associate Program Director
Jared Dyer, MD
Phone: (804) 828-9071
Email: jared.dyer@vcuhealth.org
Michael L’Heureux, MD
Phone: (804) 828-9071
Email: michael.lheureux@vcuhealth.org
Fellowship Coordinator
Abigail Sandhovel, MA
VCU School of Medicine
Department of Internal Medicine
Box 980509
Richmond, VA 23298-0509
Phone: (804) 828-9726
Email: imfellowships@vcuhealth.org
For training verification requests, please visit us at https://intmed.vcu.edu/education/verification/
