Welcome to the Sime Lab
 Welcome to the Sime Laboratory. We invite you to learn more about us from this web site and please feel free to contact us anytime. We would be pleased to hear from you.
Welcome to the Sime Laboratory. We invite you to learn more about us from this web site and please feel free to contact us anytime. We would be pleased to hear from you.
Our laboratory focuses on identifying pathogenetic mechanisms underlying lung disease so that we can speed the identification and development of new and exciting therapeutics. Diseases we study include lung scarring (fibrosis) and smoke and other toxicant induced lung inflammatory diseases such as chronic bronchitis and emphysema (COPD).
Our laboratory studies are translational in nature with our work bridging in vitro studies to in vivo models of human disease and patient studies. We have also been involved in both investigator-initiated and pharma sponsored clinical trials, and are fortunate to have been funded continuously by the NIH as well as Department of Defense, the American Lung Association, industry and philanthropy.
An important mission of the lab is to help train the next generation of basic, translational and clinical researchers. We are fortunate to collaborate widely across the institution, nationally and internationally and have a team-based approach to problem solving. Our trainees have been supported by NIH training grants including NIH T32s, F and K awards and are enjoying successful careers in academia, industry and government. Our trainees include graduate students, clinical fellows and post-doctoral fellows. All are welcome!
The Sime Lab is currently looking for graduate students, post-docs and fellows with an interest in our research. For more information contact Dr. Sime.
Research
Learn about ongoing research projects in the Sime Lab
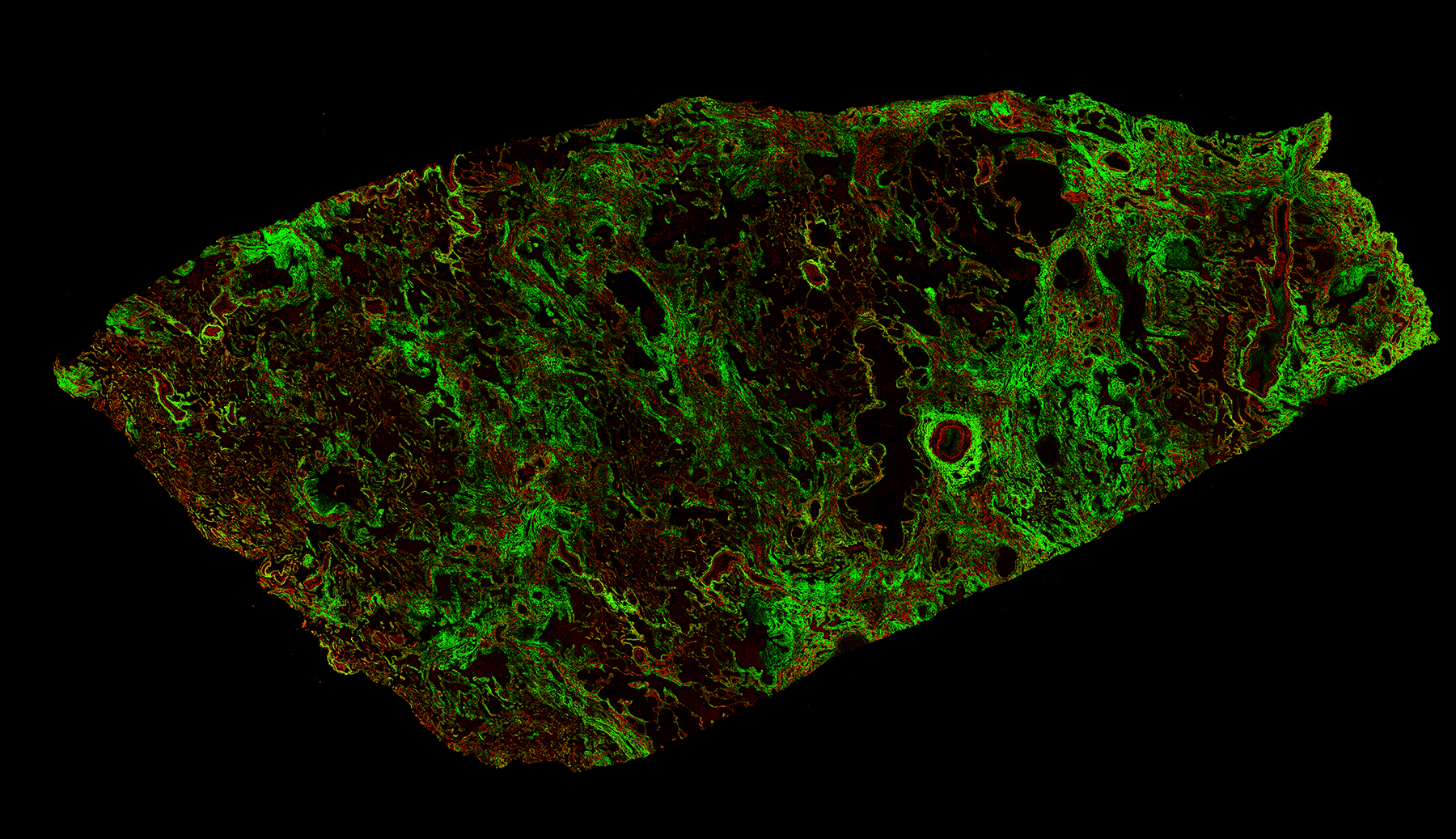
Mechanisms of Pulmonary Fibrosis
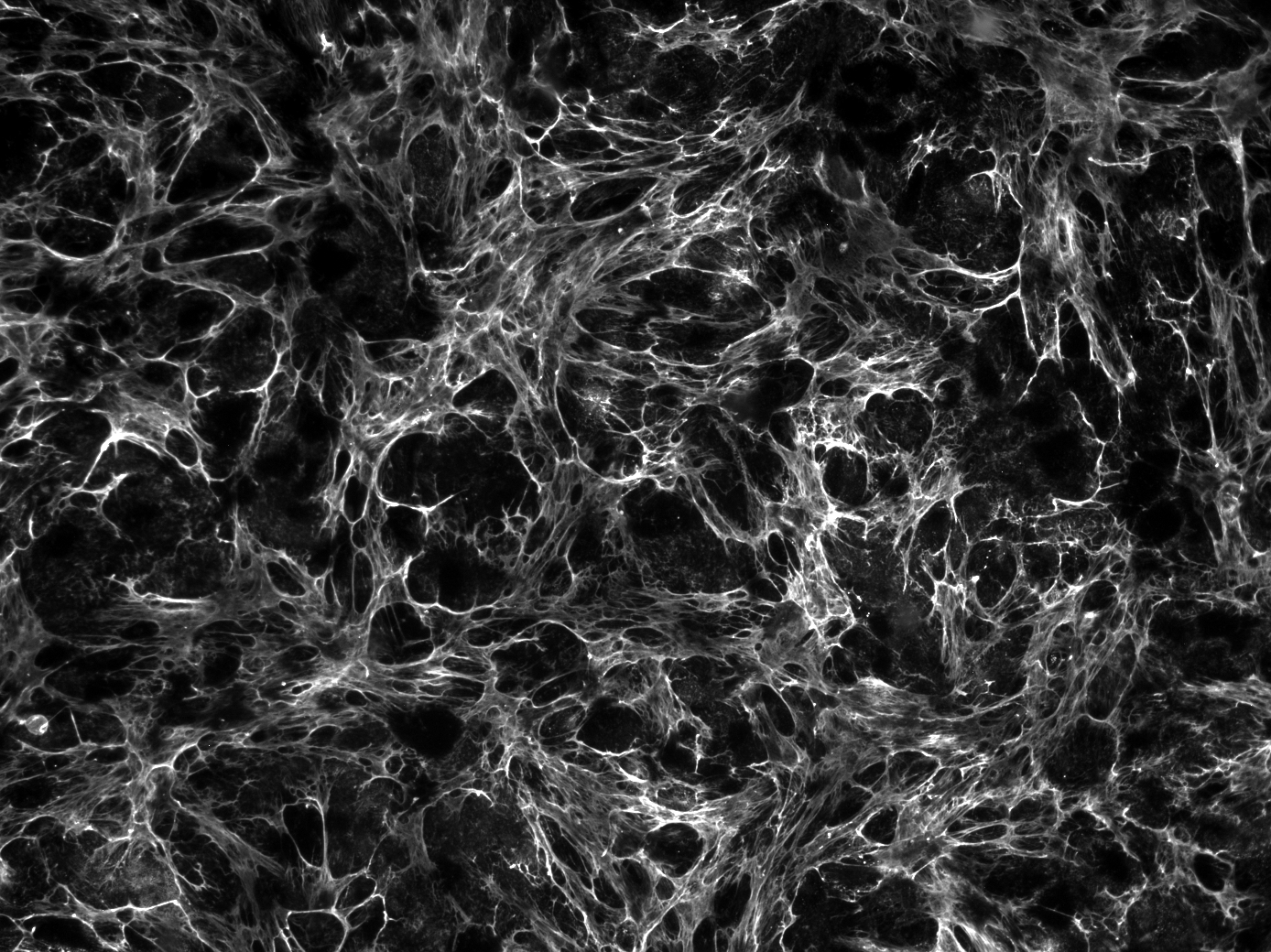
 Fibrosis (also called scarring) is estimated to be important in about 45% of human deaths. It is the result of a dysregulated uncontrolled wound healing response. When scarring occurs in vital organs the results can be devastating. Pulmonary fibrosis is a progressive disease with a shorter survival time than lung cancer. Patients with lung scarring develop shortness of breath, cough, disability and sadly sometimes succumb to these disorders. Fibrosis can occur without an identifying cause (idiopathic pulmonary fibrosis) or can be the result of dust inhalation, irradiation, exposure to toxicants and drugs and can occur with autoimmune diseases such as rheumatoid arthritis and systemic sclerosis.
Fibrosis (also called scarring) is estimated to be important in about 45% of human deaths. It is the result of a dysregulated uncontrolled wound healing response. When scarring occurs in vital organs the results can be devastating. Pulmonary fibrosis is a progressive disease with a shorter survival time than lung cancer. Patients with lung scarring develop shortness of breath, cough, disability and sadly sometimes succumb to these disorders. Fibrosis can occur without an identifying cause (idiopathic pulmonary fibrosis) or can be the result of dust inhalation, irradiation, exposure to toxicants and drugs and can occur with autoimmune diseases such as rheumatoid arthritis and systemic sclerosis.
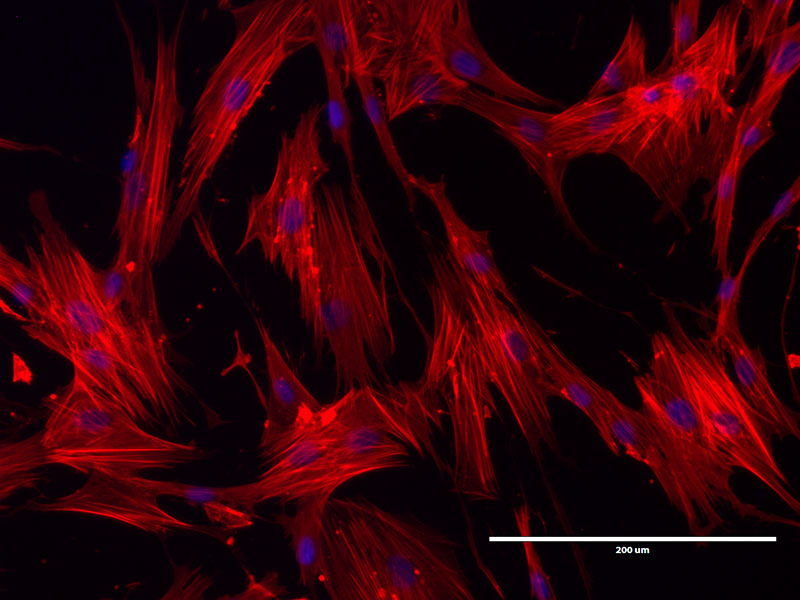
Our laboratory is NIH and industry funded to investigate the mechanisms of lung fibrosis. Specifically, we are interested in the role of matrix (the stiff glue of the scar tissue and especially cross-linking enzymes called tissue transglutaminases), abnormal metabolism (glycolysis) in cells within the lung and aspects of biomechanical tissue stiffness and stretch. To address these different aspects of fibrosis we have available primary human cells, in vivo models of disease and patient samples. We utilize cellular, genetic, lipidomic and metabolomic and physiologic approaches to interrogate pathways and collaborate with experts in big data and machine learning approaches to assist in some of the complex analyses.
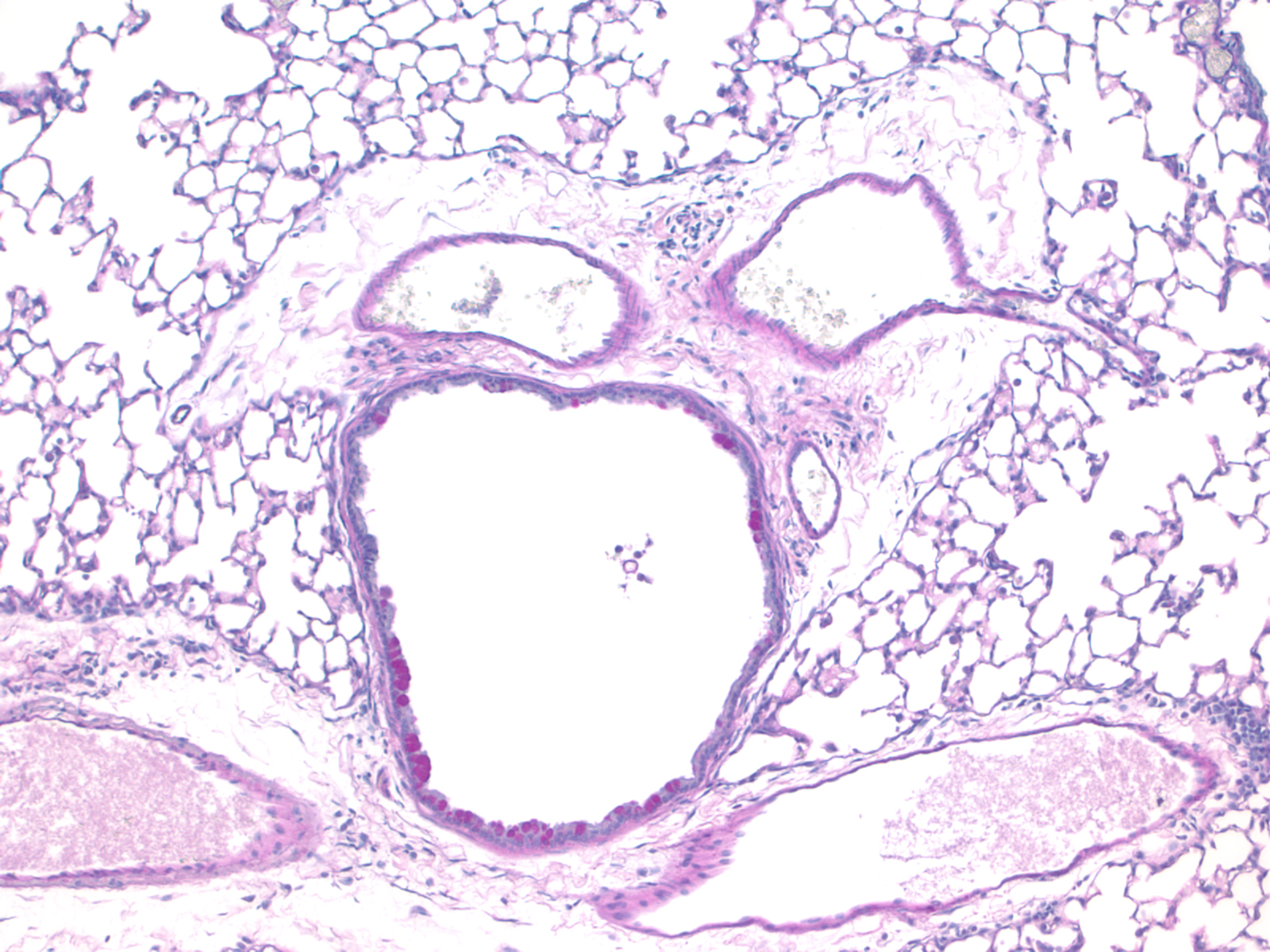
Lung Inflammation and Resolution
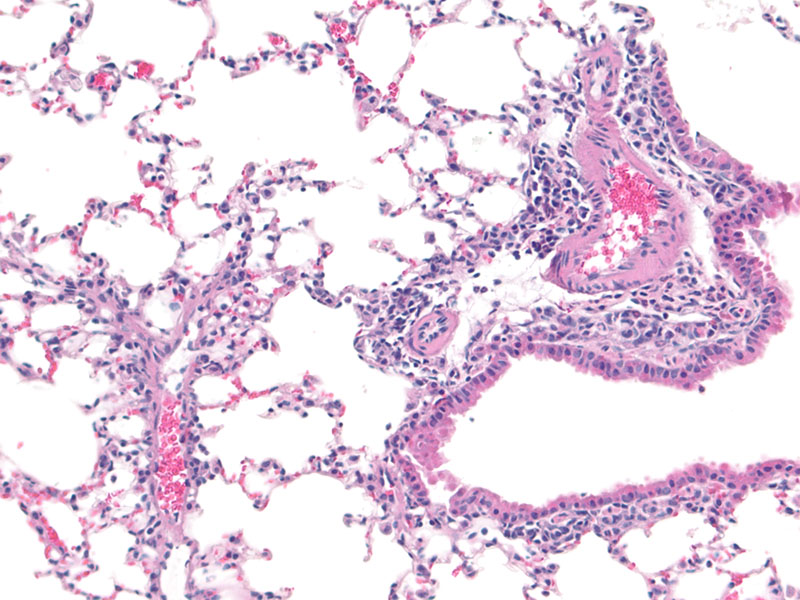 Inflammation occurs in organs following an insult and underpins much of human disease including lung diseases such as asthma, chronic obstructive pulmonary disease (COPD, chronic bronchitis and emphysema), cystic fibrosis, and some aspects of lung cancer. While we know much of the pro-inflammatory pathways that drive disease, our understanding of the resolution of inflammation is much less well understood. This is important as speeding resolution is likely an important new therapeutic option. In the last few years we have some to understand that resolution of inflammation is an active process. It requires complex cellular interactions and production of distinct mediators. Some of these mediators are derived from omega 3 and 6 fatty acids and include resolvins, protectins and maresins. We are examining how these mediators and pathways may be abnormal in patients with COPD and other lung diseases, and hypothesize that these SPMs may be exciting therapeutics for inflammatory disease. Further, we are very interested in understanding the complex interplay between lung infections, inflammation and resolution as many patients with lung disease develop infective exacerbations of their disease leading to morbidity, impaired quality of life, hospitalizations and economic costs. We use patient and control primary cells, in vivo models, pathologic assessments, physiologic measurements and state of the art lipidomics, cell biology and genetics to address our hypotheses.
Inflammation occurs in organs following an insult and underpins much of human disease including lung diseases such as asthma, chronic obstructive pulmonary disease (COPD, chronic bronchitis and emphysema), cystic fibrosis, and some aspects of lung cancer. While we know much of the pro-inflammatory pathways that drive disease, our understanding of the resolution of inflammation is much less well understood. This is important as speeding resolution is likely an important new therapeutic option. In the last few years we have some to understand that resolution of inflammation is an active process. It requires complex cellular interactions and production of distinct mediators. Some of these mediators are derived from omega 3 and 6 fatty acids and include resolvins, protectins and maresins. We are examining how these mediators and pathways may be abnormal in patients with COPD and other lung diseases, and hypothesize that these SPMs may be exciting therapeutics for inflammatory disease. Further, we are very interested in understanding the complex interplay between lung infections, inflammation and resolution as many patients with lung disease develop infective exacerbations of their disease leading to morbidity, impaired quality of life, hospitalizations and economic costs. We use patient and control primary cells, in vivo models, pathologic assessments, physiologic measurements and state of the art lipidomics, cell biology and genetics to address our hypotheses.
Our research will allow us to understand why people who smoke suffer persistent lung damage even after quitting, and to understand why smokers and ex-smokers are at increased risk of lung infection. We will also study new potential therapies to repair lung damage and restore normal immune responses. Our long-term goal is to design therapies that, in combination with quitting smoking, will improve health and reduce disease in former smokers and people exposed to second-hand and environmental smoke from other sources (Biomass and Burn Pits).
Our Team
Meet our research group

Thomas Thatcher, PhD
Assistant Professor

Thomas Thatcher, PhD
Assistant Professor
Internal Medicine
Education: PhD in Immunology, University of Rochester (2000)
Research Interests: lung inflammation and resolution
Apostolos Perelas, MD
Assistant Professor
Apostolos Perelas, MD
Assistant Professor
Internal Medicine
Division of Pulmonary Diseases and Critical Care Medicine
Phone: (804) 628-2836
Email: apostolos.perelas@vcuhealth.org
Address/Location:
Box 980050
Richmond, VA 23298

Peter Jackson, MD
Assistant Clinical Professor

Peter Jackson, MD
Assistant Clinical Professor
Internal Medicine
Division of Pulmonary Disease and Critical Care Medicine
Phone: (804) 828-9071
Email: peter.jackson@vcuhealth.org
Address/Location:
Box 980049
Richmond, VA 23298

Walker Julliard, MD
Thoracic Surgeon

Walker Julliard, MD
Thoracic Surgeon
Internal Medicine
Education: MD University of Rochester, General Surgery Residency University of Wisconsin, Postdoctoral Research Fellowship University of Wisconsin Division of Transplant Surgery, Cardiothoracic Surgery Fellowship University of Virginia
Research interests: Lung inflammation, resolution, transplant rejection, and lung cancer
Outside lab interests: Hiking, backpacking, skiing, camping, and fishing.
Email: walker.julliard@vcuhealth.org

Maggie Thomas Freeberg, PhD
Post-doctoral Research Fellow

Maggie Thomas Freeberg, PhD
Post-doctoral Research Fellow
Internal Medicine
Education: PhD and MS in Biomedical Engineering, University of Rochester, BS in Biomedical Engineering, University of Minnesota
Research Interest: Mechanotransduction mechanisms leading to pulmonary fibrosis progression
Outside Lab Interests: Outdoor adventure (hiking, kayaking, rafting, etc), cooking, board games, dogs, craft beer

Josly Pierre-Louis
PhD Candidate–Center for Clinical and Translation

Josly Pierre-Louis
PhD Candidate–Center for Clinical and Translation
Internal Medicine
Education: B.S. in Chemistry with a concentration in Biochemistry, VCU (2018); NIH PREP Scholar, VCU (2019)
Research interest: Radiation and Metabolic Mechanisms leading to Pulmonary Fibrosis
Outside lab interest: Salsa, Food Enthusiast, Sister Sister, Famille et Zanmi
Email: pierrelouisj2@vcu.edu

Yu Par Aung Myo
MD/PhD Candidate – Microbiology/Immunology

Yu Par Aung Myo
MD/PhD Candidate – Microbiology/Immunology
Internal Medicine
Education: B.S. Biology, Chemistry minor, Virginia Commonwealth University (VCU)
Research Interest: Specialized pro-resolving mediators (SPMs) in inflammation resolution in Chronic Obstructive Pulmonary Disease (COPD)
Outside Lab Interest: Painting, making jewelry, swimming, biking and learning more about nutrition
Email: myoypa@vcu.edu

Barbara Szomju
Senior Lab Technician

Barbara Szomju
Senior Lab Technician
Internal Medicine

Sarah Camus
Senior Lab Technician

Sarah Camus
Senior Lab Technician
Internal Medicine
Education: B.S. in Biology, Virginia Commonwealth University
Outside Lab Interest: baking, painting, traveling, and visiting new places in RV
Email: sarah.camus@vcuhealth.org

Jennifer Dickerson
Program Administrator Executive Assistant to Patricia J. Sime, MD, FRCP, FACP, ATSF – Chair, Department of Internal Medicine

Jennifer Dickerson
Program Administrator Executive Assistant to Patricia J. Sime, MD, FRCP, FACP, ATSF – Chair, Department of Internal Medicine
Internal Medicine
Alumni
Graduate Students at the University of Rochester: (PhD mentor unless otherwise noted)
- Ramil Sapinoro: 2001-2002
- Heather Burgess: (MSc) 2002-2004
- Randi Potter: 2003
- Pauline Chugh: 2004
- Heather Lakatos-Ferguson: 2005-2008
- Jennifer Head: 2007-2009
- David McMillan: (MSc) 2007-2010
- Christopher Hogan: 2008-2009
- Keith Olsen: (MD/PhD) 2008-2011
- HsiMin Hsiao: 2010-2015
- Amali Epa: 2011-2015
- Amanda Croasdell: 2011-2016
- Claire McCarthy: 2011-2017
- Jennifer Judge: 2012-2017
- Parker Duffney: 2012-2018
- Lindsay Wahl: 2013-2015
- Shannon Lacy: 2014-2017
- Ashley Rackow: 2017-2019
- Abdul Karim Embong: 2018-2019
- Tyler Bell: 2018-2019
- Mackenzie Palmer: 2018-2019
Post-doctoral fellows at the University of Rochester: (PhD)
- Ajit Kulkarni, PhD: 2007-2013
- Samira Kiani, MD: 2008-2009
- Ramil Sapinoro, PhD: 2008-2009
Undergraduates:
- Elizabeth Levy: (2009-2012)
- Shikha Gupta: (2009-2010)
- Robert Fulton: (2010-2011)
- Adelaide Weidner: (2018)
Clinical Trainees:
- Kate O’Reilly, MD: (2001-2002)
- Matt Lowry, MD: (2001-2003)
- Jin Yang, MD: (2001-2003)
- Louis Eugene Daugherty, MD: (2002-2004)
- R. Mathew Kottmann, MD, MS-CTR: (2005-2007)
- Michael Gurell, MD: (2007-2009)
- Rami Salibi, MD: (2011- 2012)
- Ramzy Hourany, MD: (2011-2012)
- Justin Weis, MD: (2012-2014)
- Deirdre Colgan, MD: (2013-2016)
Sime Lab
Publications
- Quenching the fires: Pro-resolving mediators, air pollution, and smoking.
Thatcher TH, Woeller CF, McCarthy CE, Sime PJ
Pharmacol Ther. 2019 May;197:212-224. doi: 10.1016/j.pharmthera.2019.02.001. Epub 2019 Feb 10. Review.
PMID: 30759375
- Key roles for lipid mediators in the adaptive immune response.
Duffney PF, Falsetta ML, Rackow AR, Thatcher TH, Phipps RP, Sime PJ
J Clin Invest. 2018 Jul 2;128(7):2724-2731. doi: 10.1172/JCI97951. Epub 2018 Jul 2. Review.
PMID: 30108196
- Prevention and treatment of bleomycin-induced pulmonary fibrosis with the lactate dehydrogenase inhibitor gossypol.
Judge JL, Nagel DJ, Owens KM, Rackow A, Phipps RP, Sime PJ, Kottmann RM.
PLoS One. 2018 May 24;13(5):e0197936. doi: 10.1371/journal.pone.0197936. eCollection 2018.
PMID: 29795645
- Activated Human Lung Fibroblasts Produce Extracellular Vesicles with Antifibrotic Prostaglandins.
Lacy SH, Woeller CF, Thatcher TH, Pollock SJ, Small EM, Sime PJ, Phipps RP.
Am J Respir Cell Mol Biol. 2019 Mar;60(3):269-278. doi: 10.1165/rcmb.2017-0248OC.
PMID: 30265126
- Secondhand Smoke Induces Inflammation and Impairs Immunity to Respiratory Infections.
Bhat TA, Kalathil SG, Bogner PN, Miller A, Lehmann PV, Thatcher TH, Phipps RP, Sime PJ, Thanavala Y.
J Immunol. 2018 Apr 15;200(8):2927-2940. doi: 10.4049/jimmunol.1701417. Epub 2018 Mar 19.
PMID: 29555783
- An Official American Thoracic Society Workshop Report: Use of Animal Models for the Preclinical Assessment of Potential Therapies for Pulmonary Fibrosis.
Jenkins RG, Moore BB, Chambers RC, Eickelberg O, Königshoff M, Kolb M, Laurent GJ, Nanthakumar CB, Olman MA, Pardo A, Selman M, Sheppard D, Sime PJ, Tager AM, Tatler AL, Thannickal VJ, White ES; ATS Assembly on Respiratory Cell and Molecular Biology.
Am J Respir Cell Mol Biol. 2017 May;56(5):667-679. doi: 10.1165/rcmb.2017-0096ST.
PMID: 28459387
- Dung biomass smoke activates inflammatory signaling pathways in human small airway epithelial cells.
McCarthy CE, Duffney PF, Gelein R, Thatcher TH, Elder A, Phipps RP, Sime PJ.
Am J Physiol Lung Cell Mol Physiol. 2016 Dec 1;311(6):L1222-L1233. doi: 10.1152/ajplung.00183.2016. Epub 2016 Nov 11.
PMID: 27836898
- Resolvin D1 Reduces Emphysema and Chronic Inflammation.
Hsiao HM, Thatcher TH, Colas RA, Serhan CN, Phipps RP, Sime PJ.
Am J Pathol. 2015 Dec;185(12):3189-201. doi: 10.1016/j.ajpath.2015.08.008. Epub 2015 Oct 24.
PMID: 26468975
- Pharmacologic inhibition of lactate production prevents myofibroblast differentiation.
Kottmann RM, Trawick E, Judge JL, Wahl LA, Epa AP, Owens KM, Thatcher TH, Phipps RP, Sime PJ.
Am J Physiol Lung Cell Mol Physiol. 2015 Dec 1;309(11):L1305-12. doi: 10.1152/ajplung.00058.2015. Epub 2015 Sep 25.
PMID: 26408551
- Inhibition of transglutaminase 2, a novel target for pulmonary fibrosis, by two small electrophilic molecules.
Olsen KC, Epa AP, Kulkarni AA, Kottmann RM, McCarthy CE, Johnson GV, Thatcher TH, Phipps RP, Sime PJ.
Am J Respir Cell Mol Biol. 2014 Apr;50(4):737-47. doi: 10.1165/rcmb.2013-0092OC.
PMID: 24175906
Dr. Sime’s complete bibliography at MyNCBI (selected from 184 total publications)
Link: https://www.ncbi.nlm.nih.gov/myncbi/patricia.sime.1/bibliography/public/
Support
Learn more about funding and collaborations
The Sime Lab has ongoing collaborations with other research teams around the world and in Virginia, including George Mason University and Fairfax Inova Hospital. Our funding sources include the National Institutes of Health, Industry, Philanthropy and Private Foundations. We gratefully acknowledge the support and friendship of the Pulmonary Fibrosis Foundation and our patients and their families, who make our research meaningful.
 |  |
|---|
.jpg)
